After reading the following cannabiz report yesterday I thought it would be worthwhile to get in touch with Aphra to dig up a little more information…
Australia: Medicinal cannabis in the crosshairs as AHPRA sets up ‘rapid response’ taskforce
The agency followed up with the following information
From a spokesperson for the Australian Health Practitioner Regulation Agency (Ahpra) to questions raised by Cannabiz
Ahpra’s traditional approach has focused on responding to individual notifications about individual health practitioners.
The Rapid Regulatory Response Unit (RRRU) is taking a problem-based approach by analysing overall issues to identify potential professional conduct concerns and harms to patients.
The Unit is proactively seeking information that will identify where practitioners are unlikely to be meeting their professional obligations and proposing responses to address the concerns.
Regulatory responses may include proposing regulatory action for individual health practitioners, referring practitioners or organisations to other regulators, or broader education-based work similar to the joint statement (see below) to ensure that all practitioners understand their obligations.
The initial areas of focus for the RRRU relate to evolving areas of the health care system with high volume and high patient demand.
- Prescription and supply of cannabis
- Prescription and supply of weight loss medication
- Prescription and supply of vaping products
- Prescription and administration of cosmetic injectables
For more information, please read the Joint statement on professional responsibilities for prescribing and dispensing medicines
Also at https://www.ahpra.gov.au/News/2024-06-03-joint-statement-prescribing-and-dispensing.aspx
The following information
Concerns raised over emerging models of care
03 Jun 2024
The emergence of services designed solely to provide customers with access to a predetermined medicine raises concerns that some practitioners may be putting profit ahead of patient welfare.
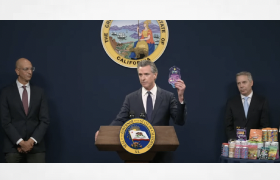
The Medical, Nursing and Midwifery and Pharmacy Boards of Australia and Ahpra are focusing on concerns that practitioners are cashing in on rising demand for the prescription and use of medicinal cannabis, bulk produced compounded medicines, or soon to be banned compounded semaglutide and related products.
Ahpra and the Boards are reminding practitioners of their long-established responsibilities when prescribing and dispensing medicines, and how they continue to apply in the context of evolving business models. A new unit will also focus on responding to practitioners who may not be complying with their codes and obligations.
Practice models of concern often feature clinics that treat a single disorder and prescribe and dispense a single medicine in response to patient demand. Some focus on a high volume of telemedicine consultations or computer or algorithm-based prescribing of medicines, and some businesses also offer direct supply of unapproved medicines to patients.
New models of healthcare, including the use of telehealth, are important enablers of greater access to health services. The Boards and Ahpra support the responsible and safe use of telehealth. The development of new medicines also plays an important role in improving the health of many patients. Ahpra and the Boards’ concerns focus only on health services and practitioners seeking to take advantage of consumer demand for certain treatments in ways that sidestep their obligations to provide safe and appropriate care.
Ahpra CEO Martin Fletcher said some emerging practices are dangerously disrupting the traditional therapeutic relationship between a patient and their practitioner.
‘Good prescribing must balance safety and access,’ Mr Fletcher said.
‘While the delivery of telehealth services is supported by Ahpra and the National Boards, we do not support practitioners or health services taking advantage of patients or ignoring their obligations to provide appropriate care and follow up when needed.
‘We remind practitioners of their duty of care when providing prescriptions of any kind, whether it be in-person or via telehealth. We also encourage consumers to be aware of these questionable practice models that are prioritising money-making over your health.’
Good practice involves a practitioner consulting with a patient, evaluating their health based on history, examination and investigations, and then recommending appropriate care based on the patient’s clinical state and the evidence supporting treatment. This includes providing patients with the range of treatment options that are available and appropriate.
Ahpra and the National Boards are seeing evidence that some health services are instead set up specifically to cater for patients who contact them seeking access to a single pre-determined medicine. Prescribers in these businesses may not be turning their minds to whether the medicine being offered is a safe or appropriate option. These medicines are then typically provided directly by a pharmacist linked to the same business.
There have also been claims that medical certificates are being issued without appropriate real-time consultations via these business models, which may leave practitioners in breach of their professional standards. The Boards and Ahpra consider that the issuing of a medical certificate requires a clinical assessment of the patient and further management may be required. It is not merely an administrative function undertaken for a patient who is willing to pay for a certificate.
New business models have seen the use of unregistered medicinal cannabis products spiral in recent years, from around 18,000 Australian patients using products in 2019 to more than one million patients using medicinal cannabis up to January 2024, according to Therapeutic Goods Administration data.
The Medical, Nursing and Midwifery and Pharmacy Boards of Australia and Ahpra are aware of reports of potentially vulnerable practitioners, particularly inexperienced or early career practitioners, who are being misled that their practice is acceptable when it is not.
Businesses focussing on the prescription of compounded glucagon-like peptide-1 (GLP-1) receptor agonists like semaglutide and tirzepatide-like products for obesity have also multiplied in recent years, with bulk-scale manufacturing prompting a TGA ban on the compounding of these medications from October 2024.
‘These business models are structured in a way that rely on restricted medicines being prescribed and billed privately in ways that mean authorities are not informed of how many people are receiving them.
‘Of even greater concern, authorities are often not able to determine exactly what substance is being provided to customers,’ Mr Fletcher said.
‘Unfortunately, some of these emerging models may be compromising your clinical care and encouraging your practitioner to breach their code of conduct in favour of personal gain.’
Ahpra and the Boards urge patients to consider these questions when seeking care:
- Does the service provide you with the opportunity to have a real-time interaction with the practitioner?
- Is a telehealth appointment appropriate for the health service you are seeking? It is generally safest to have consulted with your practitioner in-person previously to ensure they have sufficient knowledge of your health and medication history.
- Have you checked that you’re speaking to a registered health practitioner?
- Is this health practitioner registered in Australia?
- Has the practitioner gained your informed consent in relation to your consultation? The Australian Charter of Healthcare Rights includes protections for your privacy, right to confidentiality, billing or handover arrangements to inform other relevant health practitioners of the healthcare you received.
- If you are consulting virtually and haven’t previously consulted in-person, has your practitioner conducted a full assessment? For example, have they asked you about your current condition or relevant past health and medication history?
- Has your health practitioner explained to you their clinical findings, the reasons for certain treatment and any potential side effects and risks?
More information
- Read the joint statement on professional responsibilities for prescribing and dispensing medicines.
- Information for people about virtual care.
- We encourage practitioners to reach out to their insurers or professional associations for further advice.